Constipation and Periods
Constipation and periods have a well-documented link, with many experiencing sluggish bowel movements before, during, or after menstruation due to hormonal fluctuations. The experience can differ from one cycle to the next, but research shows there is a biological rationale behind these changes.
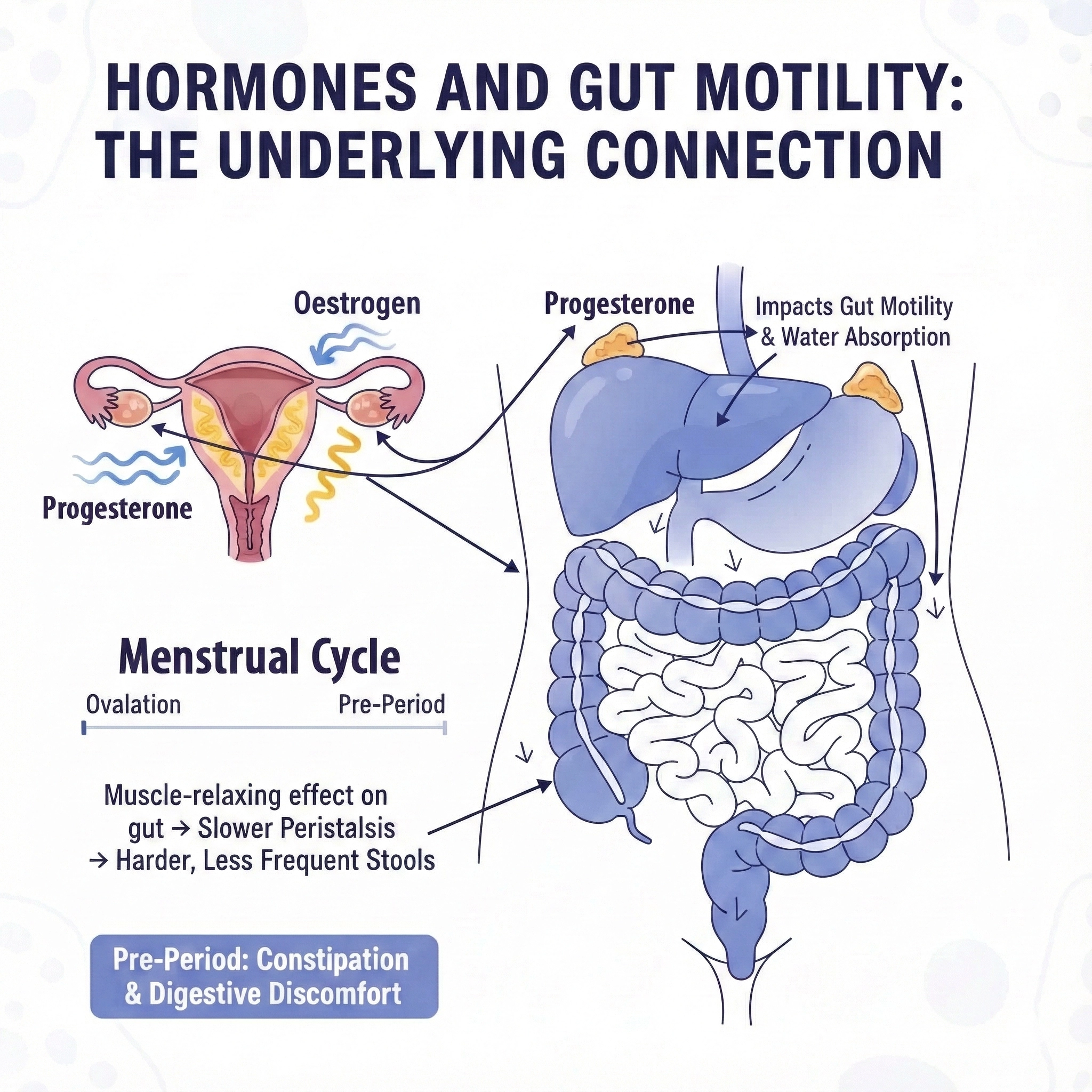
Hormones and Gut Motility:
The Underlying Connection
During the menstrual cycle, levels of oestrogen and progesterone shift markedly. After ovulation, progesterone rises to prepare the body for a possible pregnancy. This hormone has a muscle-relaxing effect, including on the gut. As a result, peristalsis, or the coordinated contractions that move stool through the intestines, slows down, causing stools to become harder and less frequent just before your period begins. Some researchers have noted that oestrogen, which peaks before menstruation, may also impact gut motility and water absorption in the colon, compounding the problem for some individuals.
Constipation Before, During, and After Periods
Premenstrual constipation typically occurs as progesterone surges after ovulation. The gut’s muscle contractions are dampened, stool spends longer in the colon, and more water is absorbed resulting in harder, drier stools. It is not unusual to notice heightened bloating, abdominal pain, and the sensation of incomplete emptying at this stage in the cycle. If other factors such as low dietary fibre, dehydration, or less physical activity coincide, symptoms may worsen.
Once menstruation begins, hormone levels, particularly progesterone, drop sharply. For many, this brings a return to normal bowel movement frequency, yet for others, symptoms such as constipation or bloating persist through the period itself. Factors like stress, dietary changes, pain medication use, or heightened fluid retention can further slow gut transit. Period cramps and bowel discomfort can overlap, making constipation more painful or noticeable, and some may also experience alternating constipation and diarrhoea due to prostaglandin fluctuations in the uterus and bowel tissue.
Most experience an improvement in bowel function once the period concludes and the hormonal roller coaster stabilises for the following couple of weeks. However, if dietary fibre and hydration are lacking, or if underlying gut sensitivity remains, occasional sluggishness or incomplete emptying can persist. Each person’s recovery timeline varies, but extended constipation after a period may signal a need for medical advice or changes in routine.
Practical Remedies and Gentle Support

The Natural Power of Green Kiwifruit
Kiwi stands out among digestive aids for supporting gentle, effective regularity during hormonal shifts. Clinical data confirms that eating two green kiwifruit or using equivalent supplement forms reliably increases stool frequency and softens stool consistency for those experiencing constipation. Actazin®, derived from New Zealand’s Hayward green kiwifruit, brings together insoluble and soluble fibre, water-retention capacity, and the enzyme actinidin to aid healthy transit. Aside from promoting regular bowel activity, kiwifruit is mild, supportive, and suitable for those with sensitive digestion.

Final Thoughts
Digestive changes through the menstrual cycle are normal but can affect wellbeing. Constipation before, during, or after periods is primarily linked to hormonal shifts—slowing gut motility and changing how the gut handles water and nutrients. Consistent hydration, a fibre-rich diet, and movement are practical strategies for lasting comfort. For natural, science-backed support, green kiwifruit and supplements like Actazin offer a gentle solution to both routine and hormone-driven constipation, celebrating New Zealand’s tradition of health from the inside out. If constipation lingers for more than two weeks, or severe pain or bleeding occurs, consult a healthcare professional for further advice.





